Oral & Maxillofacial Surgery
What is Oral & Maxillofacial Surgery?
Oral and maxillofacial surgery is that specialty which involves the diagnosis, surgical and medical treatment of diseases, injuries, deformities, and defects of the mouth, jaws and facial region.
Our Oral and Maxillofacial Surgeon, Dr. Akbar Lightbourne, treats and cares for patients in office as well as in King Edward Memorial Hospital.
Oral and maxillofacial surgery is that specialty which involves the diagnosis, surgical and medical treatment of diseases, injuries, deformities, and defects of the mouth, jaws and facial region.
Our Oral and Maxillofacial Surgeon, Dr. Akbar Lightbourne, treats and cares for patients in office as well as in King Edward Memorial Hospital.

Tooth Extraction
What is a wisdom tooth?
Tooth extraction is the surgical removal of a tooth from the jaw and mouth. There are many reasons why an individual would choose to remove their teeth ranging from pain, decay, pathology, infection, misalignment and crowding.
Whatever the case may be, Dr. Lightbourne will assist you in providing treatment in a manner that is the most comfortable for you.
What is a wisdom tooth?
Tooth extraction is the surgical removal of a tooth from the jaw and mouth. There are many reasons why an individual would choose to remove their teeth ranging from pain, decay, pathology, infection, misalignment and crowding.
Whatever the case may be, Dr. Lightbourne will assist you in providing treatment in a manner that is the most comfortable for you.

Third Molars
What is a wisdom tooth?
Wisdom teeth are the third molars and are typically the last teeth to erupt within the mouth. When they align properly and gum tissue is healthy, wisdom teeth do not have to be removed. Unfortunately, this does not generally happen. The extraction of wisdom teeth is necessary when they become impacted and are prevented from properly erupting within the mouth.
What is an impacted wisdom tooth?
A tooth becomes impacted when there is a lack of space in the dental arch and its growth and eruption are prevented by overlying gum, bone or another tooth. A tooth may be partially impacted, which means a portion of it has broken through the gum, or totally impacted and unable to break through the gum at all.
Should I have my wisdom teeth removed?
Impacted and partially impacted teeth can be painful and lead to infection. They may also crowd or damage adjacent teeth or roots. More serious problems may occur if the sac surrounding the impacted tooth becomes filled with fluid and enlarges to form a cyst. As the cyst grows it may hollow out the jaw and permanently damage adjacent teeth, the surrounding bone and nerves. Rarely, if a cyst is not treated, a tumor may develop from its walls and a more serious surgical procedure may be required to remove it. Complications may arise from partially impacted teeth and totally impacted teeth.
Recommended age for removal
It isn't wise to wait until your wisdom teeth start to bother you. In general, earlier removal of wisdom teeth results in a less complicated healing process.
Wisdom teeth are easier to remove when the patient is younger, since their roots are not completely formed, the surrounding bone is softer, and there is less chance of damaging nearby nerves or other structures. Removal of wisdom teeth at a later age becomes more complicated as the roots have fully developed (may involve the nerve), and the jawbone is denser.
What is a wisdom tooth?
Wisdom teeth are the third molars and are typically the last teeth to erupt within the mouth. When they align properly and gum tissue is healthy, wisdom teeth do not have to be removed. Unfortunately, this does not generally happen. The extraction of wisdom teeth is necessary when they become impacted and are prevented from properly erupting within the mouth.
What is an impacted wisdom tooth?
A tooth becomes impacted when there is a lack of space in the dental arch and its growth and eruption are prevented by overlying gum, bone or another tooth. A tooth may be partially impacted, which means a portion of it has broken through the gum, or totally impacted and unable to break through the gum at all.
Should I have my wisdom teeth removed?
Impacted and partially impacted teeth can be painful and lead to infection. They may also crowd or damage adjacent teeth or roots. More serious problems may occur if the sac surrounding the impacted tooth becomes filled with fluid and enlarges to form a cyst. As the cyst grows it may hollow out the jaw and permanently damage adjacent teeth, the surrounding bone and nerves. Rarely, if a cyst is not treated, a tumor may develop from its walls and a more serious surgical procedure may be required to remove it. Complications may arise from partially impacted teeth and totally impacted teeth.
Recommended age for removal
It isn't wise to wait until your wisdom teeth start to bother you. In general, earlier removal of wisdom teeth results in a less complicated healing process.
Wisdom teeth are easier to remove when the patient is younger, since their roots are not completely formed, the surrounding bone is softer, and there is less chance of damaging nearby nerves or other structures. Removal of wisdom teeth at a later age becomes more complicated as the roots have fully developed (may involve the nerve), and the jawbone is denser.
Dental Implants
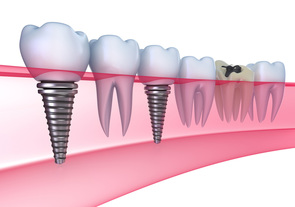
Dental implants are changing the way people live. Designed to provide a foundation for replacement teeth that look, feel, and function like natural teeth. An individual who has lost teeth is able to regain the ability to eat virtually anything, knowing that teeth appear natural and that facial contours will be preserved. Patients with dental implants can smile with confidence.
What is a Dental Implant?
A dental implant is a tooth root analogue (replica). It is an artificial tooth root made of surgical grade titanium, which is placed into the jaw onto which crowns and bridgework can be constructed.
Dental implants have numerous possible applications in dentistry:
Are you a candidate for dental implants?
If you are considering dental implants, Dr. Lightbourne will work with you and your dentist to determine how dental implants can be used for your specific case. Following an initial consultation Dr. Lightbourne will address your specific needs and considerations and develop a treatment plan tailored just for you.
Dental implants are changing the way people live. Designed to provide a foundation for replacement teeth that look, feel, and function like natural teeth. An individual who has lost teeth is able to regain the ability to eat virtually anything, knowing that teeth appear natural and that facial contours will be preserved. Patients with dental implants can smile with confidence.
What is a Dental Implant?
A dental implant is a tooth root analogue (replica). It is an artificial tooth root made of surgical grade titanium, which is placed into the jaw onto which crowns and bridgework can be constructed.
Dental implants have numerous possible applications in dentistry:
- To replace a single or multiple teeth without affecting adjacent teeth
- To support bridgework or replace a partial denture
- To help support or secure upper or lower dentures
Are you a candidate for dental implants?
If you are considering dental implants, Dr. Lightbourne will work with you and your dentist to determine how dental implants can be used for your specific case. Following an initial consultation Dr. Lightbourne will address your specific needs and considerations and develop a treatment plan tailored just for you.
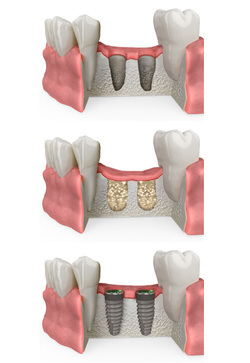
Bone Graft
Over a period of time, the jaw bone associated with missing teeth, begins to resorb as the result of the lack of function, periodontal disease or trauma. This often leaves a condition in which there is poor quality and quantity of bone suitable for placement of dental implants in the required location. Bone grafting is a surgical procedure that replaces missing bone with either new bone from the patient's own body, with a natural bone substitute or with a synthetic graft material.
Reasons for bone graftingThere are a wide variety of reasons why bone grafting may be the best option for restoring the jaw bone.
Dental implants - Implants are the preferred replacement method for missing teeth because they restore full functionality to the mouth; however, implants need to be firmly anchored to the jawbone to be effective. If the jawbone lacks the necessary quality or quantity of bone, bone grafting can strengthen and thicken the tooth site to allow future implant placement.
Ridge augmentation - Ridges in the bone can occur due to trauma, injury, birth defects or severe periodontal disease. The bone graft is used to fill in the ridge and make the jawbone a uniform shape.
Pathology - Pathologic lesions that develop within the bone can resorb vital bone structure that gives strength to the jaw bone and supports the teeth. When these lesions are removed bone grafting is done to replace this deficient bone to support the jaw bone and teeth together.
What Does Bone Grafting Involve?
Bone grafting can either be completed in-office or scheduled for the hospital as a same day procedure. Bone is typically harvested from your own body (or on rare occasions obtained from a bone bank) and added to the affected site. This natural bone is taken from within your mouth for smaller grafting needs or from your hip or lateral knee for larger more involved requirements. The bone graft fills in the missing bone but also stimulates the growth of your own bone that acts as a strengthening bridge between the graft and your existing bone. The bone graft is then allowed to heal in the new location over a period of a few months. Over time, most of the graft material will be replaced by your own newly formed bone.
Over a period of time, the jaw bone associated with missing teeth, begins to resorb as the result of the lack of function, periodontal disease or trauma. This often leaves a condition in which there is poor quality and quantity of bone suitable for placement of dental implants in the required location. Bone grafting is a surgical procedure that replaces missing bone with either new bone from the patient's own body, with a natural bone substitute or with a synthetic graft material.
Reasons for bone graftingThere are a wide variety of reasons why bone grafting may be the best option for restoring the jaw bone.
Dental implants - Implants are the preferred replacement method for missing teeth because they restore full functionality to the mouth; however, implants need to be firmly anchored to the jawbone to be effective. If the jawbone lacks the necessary quality or quantity of bone, bone grafting can strengthen and thicken the tooth site to allow future implant placement.
Ridge augmentation - Ridges in the bone can occur due to trauma, injury, birth defects or severe periodontal disease. The bone graft is used to fill in the ridge and make the jawbone a uniform shape.
Pathology - Pathologic lesions that develop within the bone can resorb vital bone structure that gives strength to the jaw bone and supports the teeth. When these lesions are removed bone grafting is done to replace this deficient bone to support the jaw bone and teeth together.
What Does Bone Grafting Involve?
Bone grafting can either be completed in-office or scheduled for the hospital as a same day procedure. Bone is typically harvested from your own body (or on rare occasions obtained from a bone bank) and added to the affected site. This natural bone is taken from within your mouth for smaller grafting needs or from your hip or lateral knee for larger more involved requirements. The bone graft fills in the missing bone but also stimulates the growth of your own bone that acts as a strengthening bridge between the graft and your existing bone. The bone graft is then allowed to heal in the new location over a period of a few months. Over time, most of the graft material will be replaced by your own newly formed bone.

Sinus Lift
The maxillary sinuses are air filled cavities within the upper jaw that sit above the upper teeth. When these upper teeth are removed, there is often just a thin wall of bone separating the maxillary sinus and the mouth. If you are looking at dental implants as a solution to replace missing teach this can be a potential limiting factor as implants need enough bone to hold them in place. When the sinus wall is very thin, it is impossible to place dental implants in this bone.
A sinus lift surgery is a solution to this problem. By raising the sinus floor upwards and placing in bone into the newly created space this creates a sufficient bony height for future implant placement. The sinus graft makes it possible for many patients to have dental implants when years ago there was no other option than wearing loose dentures.
If enough bone between the upper jaw ridge and the bottom of the sinus is available to stabilize the implant well, sinus augmentations and implant placement can sometimes be performed as a single procedure. If not enough bone is available, the sinus augmentation will have to be performed first, then the graft will have to mature for several months. Once the graft has matured, the implants can be placed.
The maxillary sinuses are air filled cavities within the upper jaw that sit above the upper teeth. When these upper teeth are removed, there is often just a thin wall of bone separating the maxillary sinus and the mouth. If you are looking at dental implants as a solution to replace missing teach this can be a potential limiting factor as implants need enough bone to hold them in place. When the sinus wall is very thin, it is impossible to place dental implants in this bone.
A sinus lift surgery is a solution to this problem. By raising the sinus floor upwards and placing in bone into the newly created space this creates a sufficient bony height for future implant placement. The sinus graft makes it possible for many patients to have dental implants when years ago there was no other option than wearing loose dentures.
If enough bone between the upper jaw ridge and the bottom of the sinus is available to stabilize the implant well, sinus augmentations and implant placement can sometimes be performed as a single procedure. If not enough bone is available, the sinus augmentation will have to be performed first, then the graft will have to mature for several months. Once the graft has matured, the implants can be placed.
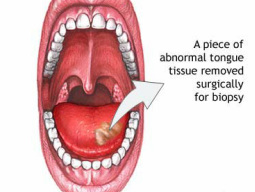
Biopsy (Oral Pathology)
The inside of the mouth is normally lined with a special type of skin (mucosa) that is smooth and coral pink in color. Any alteration in this appearance could be a warning sign for a pathological process. The most serious of these is oral cancer. The following can be signs at the beginning of a pathologic process or cancerous growth:
We would recommend performing an oral cancer self-examination monthly and remember that your mouth is one of your body's most important warning systems. Do not ignore suspicious lumps or sores. Please contact us so we may help.
The inside of the mouth is normally lined with a special type of skin (mucosa) that is smooth and coral pink in color. Any alteration in this appearance could be a warning sign for a pathological process. The most serious of these is oral cancer. The following can be signs at the beginning of a pathologic process or cancerous growth:
- Reddish patches (erythroplasia) or whitish patches (leukoplakia) in the mouth.
- A sore that fails to heal and bleeds easily.
- A lump or thickening on the skin lining the inside of the mouth.
- Chronic sore throat or hoarseness. Difficulty in chewing or swallowing.
We would recommend performing an oral cancer self-examination monthly and remember that your mouth is one of your body's most important warning systems. Do not ignore suspicious lumps or sores. Please contact us so we may help.

Facial Trauma
Injury to Face, Mouth and Teeth
Oral and maxillofacial surgeons are trained, skilled and uniquely qualified to manage and treat facial trauma. Injuries to the face, by their very nature, impart a high degree of emotional, as well as physical trauma to patients.
The science and art of treating these injuries requires special training involving a "hands on" experience and an understanding of how the treatment provided will influence the patient's long term function and appearance.
Dr. Lightbourne meets and exceeds these modern standards. He is trained, skilled, and uniquely qualified to manage and treat facial trauma. He is on staff at King Edward Memorial Hospital and delivers emergency room coverage for facial injuries, which include the following conditions:
The Nature Of Maxillofacial Trauma
There are a number of possible causes of facial trauma such as motor vehicle accidents, accidental falls, sports injuries, interpersonal violence, and work-related injuries. Types of facial injuries can range from injuries of teeth to extremely severe injuries of the skin and bones of the face. Typically, facial injuries are classified as either soft tissue injuries (skin and gums), bone injuries (fractures), or injuries to special regions (such as the eyes, facial nerves or the salivary glands).
Soft Tissue Injuries Of The Maxillofacial Region
When soft tissue injuries such as lacerations occur on the face, they are repaired by suturing. In addition to the obvious concern of providing a repair that yields the best cosmetic result possible, care is taken to inspect for and treat injuries to structures such as facial nerves, salivary glands, and salivary ducts (or outflow channels). Dr. Lightbourne is a well-trained oral and maxillofacial surgeon and is proficient at diagnosing and treating all types of facial lacerations.
Bone Injuries Of The Maxillofacial Region
Fractures of the bones of the face are treated in a manner similar to the fractures in other parts of the body. The specific form of treatment is determined by various factors, which include the location of the fracture, the severity of the fracture, the age, and general health of the patient. When an arm or a leg is fractured, a cast is often applied to stabilize the bone to allow for proper healing. Since a cast cannot be placed on the face, other means have been developed to stabilize facial fractures.
One of these options involves wiring the jaws together for certain fractures of the upper and/or lower jaw. Certain other types of fractures of the jaw are best treated and stabilized by the surgical placement of small plates and screws at the involved site. This technique of treatment can often allow for healing and obviates the necessity of having the jaws wired together. This technique is called "rigid fixation" of a fracture. The relatively recent development and use of rigid fixation has profoundly improved the recovery period for many patients, allowing them to return to normal function more quickly.
The treatment of facial fractures should be accomplished in a thorough and predictable manner. More importantly, the patient's facial appearance should be minimally affected. An attempt at accessing the facial bones through the fewest incisions necessary is always made. At the same time, the incisions that become necessary, are designed to be small and, whenever possible, are placed so that the resultant scar is hidden.
Injuries To The Teeth & Surrounding Dental Structures
Isolated injuries to teeth are quite common and may require the expertise of various dental specialists. Oral surgeons usually are involved in treating fractures in the supporting bone or in replanting teeth that have been displaced or knocked out. These types of injuries are treated by one of a number of forms of splinting (stabilizing by wiring or bonding teeth together). If a tooth is knocked out, it should be placed in salt water or milk. The sooner the tooth is re-inserted into the dental socket, the better chance it will survive. Therefore, the patient should see a dentist or oral surgeon as soon as possible. Never attempt to wipe the tooth off, since remnants of the ligament that hold the tooth in the jaw are attached and are vital to the success of replanting the tooth. Other dental specialists may be called upon such as endodontists, who may be asked to perform root canal therapy, and/or restorative dentists who may need to repair or rebuild fractured teeth. In the event that injured teeth cannot be saved or repaired, dental implants are often now utilized as replacements for missing teeth.
The proper treatment of facial injuries is now the realm of specialists who are well versed in emergency care, acute treatment, long-term reconstruction, and rehabilitation of the patient.
Injury to Face, Mouth and Teeth
Oral and maxillofacial surgeons are trained, skilled and uniquely qualified to manage and treat facial trauma. Injuries to the face, by their very nature, impart a high degree of emotional, as well as physical trauma to patients.
The science and art of treating these injuries requires special training involving a "hands on" experience and an understanding of how the treatment provided will influence the patient's long term function and appearance.
Dr. Lightbourne meets and exceeds these modern standards. He is trained, skilled, and uniquely qualified to manage and treat facial trauma. He is on staff at King Edward Memorial Hospital and delivers emergency room coverage for facial injuries, which include the following conditions:
- Minor and major facial lacerations
- Intra-oral and facial infections
- Fractured facial bones (cheek, nose or eye socket)
- Fractured jaws (upper and lower jaw)
The Nature Of Maxillofacial Trauma
There are a number of possible causes of facial trauma such as motor vehicle accidents, accidental falls, sports injuries, interpersonal violence, and work-related injuries. Types of facial injuries can range from injuries of teeth to extremely severe injuries of the skin and bones of the face. Typically, facial injuries are classified as either soft tissue injuries (skin and gums), bone injuries (fractures), or injuries to special regions (such as the eyes, facial nerves or the salivary glands).
Soft Tissue Injuries Of The Maxillofacial Region
When soft tissue injuries such as lacerations occur on the face, they are repaired by suturing. In addition to the obvious concern of providing a repair that yields the best cosmetic result possible, care is taken to inspect for and treat injuries to structures such as facial nerves, salivary glands, and salivary ducts (or outflow channels). Dr. Lightbourne is a well-trained oral and maxillofacial surgeon and is proficient at diagnosing and treating all types of facial lacerations.
Bone Injuries Of The Maxillofacial Region
Fractures of the bones of the face are treated in a manner similar to the fractures in other parts of the body. The specific form of treatment is determined by various factors, which include the location of the fracture, the severity of the fracture, the age, and general health of the patient. When an arm or a leg is fractured, a cast is often applied to stabilize the bone to allow for proper healing. Since a cast cannot be placed on the face, other means have been developed to stabilize facial fractures.
One of these options involves wiring the jaws together for certain fractures of the upper and/or lower jaw. Certain other types of fractures of the jaw are best treated and stabilized by the surgical placement of small plates and screws at the involved site. This technique of treatment can often allow for healing and obviates the necessity of having the jaws wired together. This technique is called "rigid fixation" of a fracture. The relatively recent development and use of rigid fixation has profoundly improved the recovery period for many patients, allowing them to return to normal function more quickly.
The treatment of facial fractures should be accomplished in a thorough and predictable manner. More importantly, the patient's facial appearance should be minimally affected. An attempt at accessing the facial bones through the fewest incisions necessary is always made. At the same time, the incisions that become necessary, are designed to be small and, whenever possible, are placed so that the resultant scar is hidden.
Injuries To The Teeth & Surrounding Dental Structures
Isolated injuries to teeth are quite common and may require the expertise of various dental specialists. Oral surgeons usually are involved in treating fractures in the supporting bone or in replanting teeth that have been displaced or knocked out. These types of injuries are treated by one of a number of forms of splinting (stabilizing by wiring or bonding teeth together). If a tooth is knocked out, it should be placed in salt water or milk. The sooner the tooth is re-inserted into the dental socket, the better chance it will survive. Therefore, the patient should see a dentist or oral surgeon as soon as possible. Never attempt to wipe the tooth off, since remnants of the ligament that hold the tooth in the jaw are attached and are vital to the success of replanting the tooth. Other dental specialists may be called upon such as endodontists, who may be asked to perform root canal therapy, and/or restorative dentists who may need to repair or rebuild fractured teeth. In the event that injured teeth cannot be saved or repaired, dental implants are often now utilized as replacements for missing teeth.
The proper treatment of facial injuries is now the realm of specialists who are well versed in emergency care, acute treatment, long-term reconstruction, and rehabilitation of the patient.

Jaw Surgery (Orthognathic Surgery)
Orthognathic surgery is needed when teeth don't meet correctly and/or the jaws have not grown into their correct positions. The treatment is typically done working with an Orthodontist, who using braces, straightens the teeth and aligns them to come into a normal biting position for the repositioned jaw bones. This not only improves facial appearance, but also ensures that teeth meet correctly and function properly.
Who Needs Orthognathic Surgery?
People who can benefit from orthognathic surgery include those with an improper bite or jaws that are positioned incorrectly. Jaw growth is a gradual process and in some instances, the upper and lower jaws may grow at different rates. The result can be a host of problems that can affect chewing function, speech, long-term oral health and appearance. Injury to the jaw and birth defects can also affect jaw alignment. Orthodontics alone can correct bite problems when only the teeth are involved. Orthognathic surgery may be required for the jaws when repositioning is necessary.
Difficulty in the following areas should be evaluated
Technology & Orthognathic Surgery
Dr. Lightbourne uses modern computer techniques and models to show you exactly how your surgery will be approached. Using comprehensive facial x-rays and computer video imaging, we can show you how your bite will be improved and even give you an idea of how you'll look after surgery. This helps you understand the surgical process and the extent of the treatment prescribed. Our goal is to help you understand the benefits of orthognathic surgery.
If you are a candidate for corrective jaw surgery, Dr. Lightbourne will work closely with your dentist and orthodontist during your treatment. The actual surgery can move your teeth and jaws into a new position that results in a more attractive, functional, and healthy dental-facial relationship.
Orthognathic surgery is needed when teeth don't meet correctly and/or the jaws have not grown into their correct positions. The treatment is typically done working with an Orthodontist, who using braces, straightens the teeth and aligns them to come into a normal biting position for the repositioned jaw bones. This not only improves facial appearance, but also ensures that teeth meet correctly and function properly.
Who Needs Orthognathic Surgery?
People who can benefit from orthognathic surgery include those with an improper bite or jaws that are positioned incorrectly. Jaw growth is a gradual process and in some instances, the upper and lower jaws may grow at different rates. The result can be a host of problems that can affect chewing function, speech, long-term oral health and appearance. Injury to the jaw and birth defects can also affect jaw alignment. Orthodontics alone can correct bite problems when only the teeth are involved. Orthognathic surgery may be required for the jaws when repositioning is necessary.
Difficulty in the following areas should be evaluated
- Difficulty in chewing, biting or swallowing
- Speech problems
- Chronic jaw or TMJ pain
- Open bite
- Protruding jaw
- Breathing problems
Technology & Orthognathic Surgery
Dr. Lightbourne uses modern computer techniques and models to show you exactly how your surgery will be approached. Using comprehensive facial x-rays and computer video imaging, we can show you how your bite will be improved and even give you an idea of how you'll look after surgery. This helps you understand the surgical process and the extent of the treatment prescribed. Our goal is to help you understand the benefits of orthognathic surgery.
If you are a candidate for corrective jaw surgery, Dr. Lightbourne will work closely with your dentist and orthodontist during your treatment. The actual surgery can move your teeth and jaws into a new position that results in a more attractive, functional, and healthy dental-facial relationship.
